Highmark Well being, Abridge Associate to scale AI for payers/suppliers
Highmark Well being works along with Healthcare AI Firm Abridge to roll out its environmental platform for the setting of the Ambient and to develop a previous authorization answer, the businesses introduced on Tuesday.
Pittsburgh, Highmark Well being in Pennsylvania is the guardian firm of Highmark, a well being insurer with greater than 7 million members and Allegheny Well being Community, a well being system with 14 hospitals. Abridge, additionally based mostly in Pittsburgh, presents an AI platform that goals to enhance the outcomes of the affected person and cut back administrative burdens for suppliers.
By way of the partnership, the scientific intelligence platform of Abridge shall be built-in on Allegheny Well being Community Workplace places and hospitals. The platform takes conversations of patient-clinical conversations and turns them into scientific notes. After acquiring the affected person's permission, conversations are recorded utilizing a phone or pc. Scientific notes are made in actual time throughout the physician's workflow and the physician can assess and edit the notes earlier than they’re added to the affected person's EPD.
Using this know-how reduces the period of time that clinicians should spend on making notes and permits them to spend extra time with sufferers, in response to the businesses. The implementation of Abridge setting know-how begins at outpatient places, however will ultimately be utilized in the complete well being system.
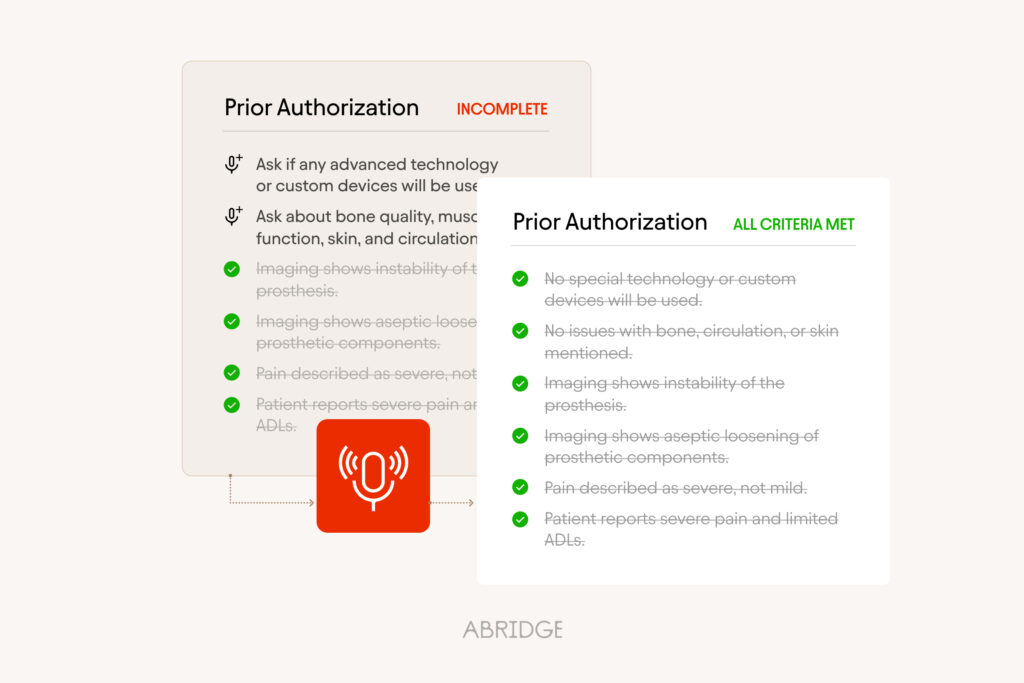
Highmark Well being and Abridge additionally work collectively on constructing a brand new prior authorization know-how. Throughout affected person visits, the know-how will establish when prior permission is required and the physician will ask for lacking data for the authorization earlier than the affected person leaves the Home.
“The platform will routinely generate the request with all the data required for approval in actual time,” Abridge spokesperson instructed MedCity Information. “The linked proof structure of Abridge permits the clinicus to seamlessly confirm every part within the AI -generated observe and the supply transcript and to request the audio from the dialog, in order that they’ll make certain that data is correct and in depth.”
This builds on the Gold Carding Program of Highmark Well being, which grants gold maps to practices and docs with a confirmed document of excessive prior permission for permission. As quickly as Gold Carded, docs solely need to submit a prenotification to plan providers and approval is instantly granted. Highmark Well being additionally presents an energetic gold card program, which signifies that Highmarkt cooperates instantly with clinicians, who presents teaching to assist them submit correct and clinically appropriate requests.
“Whereas these [gold carding] Initiatieven kunnen de eerdere autorisaties op het punt van zorg na de plaatsvondiging vergroten, de technologie van Abridge vraagt clinici naar nodige informatie tijdens patiëntenbezoeken, wat leidt tot snellere goedkeuringen en minder weigering, wat uiteindelijk helpt patiënten de continuïteit van de zorg te behouden, ”zei Richard Clarke, PhD, SVP, Chief Analytics Officer van Highmark Well being, in een e-mail, in an e-mail.
In the end, this partnership between Highmark Well being and Abridge goals to enhance well being outcomes and make the care extra reasonably priced, Clarke added.
“Sufferers may have extra face time with their docs because of the environmental author know-how that we assume [Allegheny Health Network]”He mentioned. “Comply with-up care shall be accepted extra effectively by way of the prior Auth answer. Because the collaboration ripens, we’ll search for different methods to make use of AI instruments and options creatively inside our present workflows, and through the care continuum.”
Photograph: Abridge and Highmark Well being