
OIG is insisting on stronger ensures as a distant invoicing will increase in affected person monitoring
As dwelling care suppliers more and more undertake exterior affected person monitoring (RPM), watchdogs improve the investigation into potential fraud in invoicing for these providers.
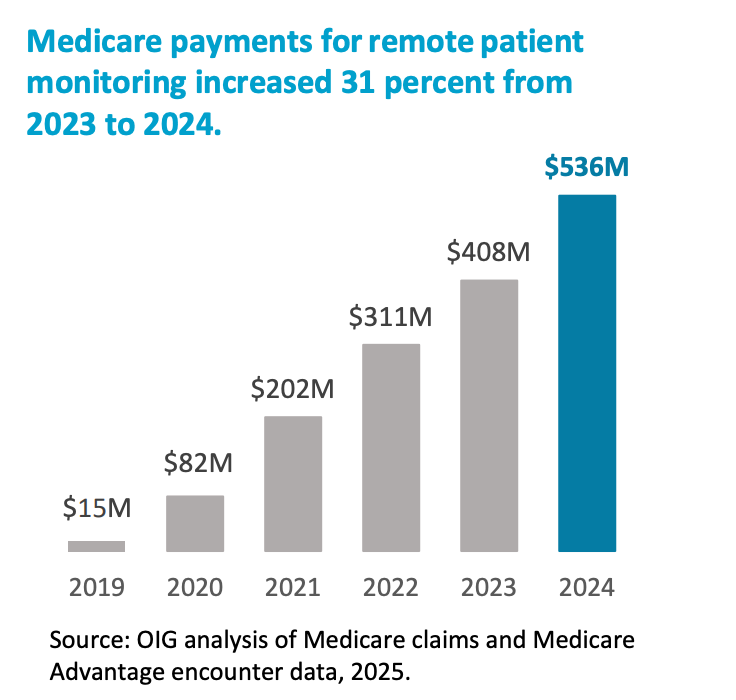
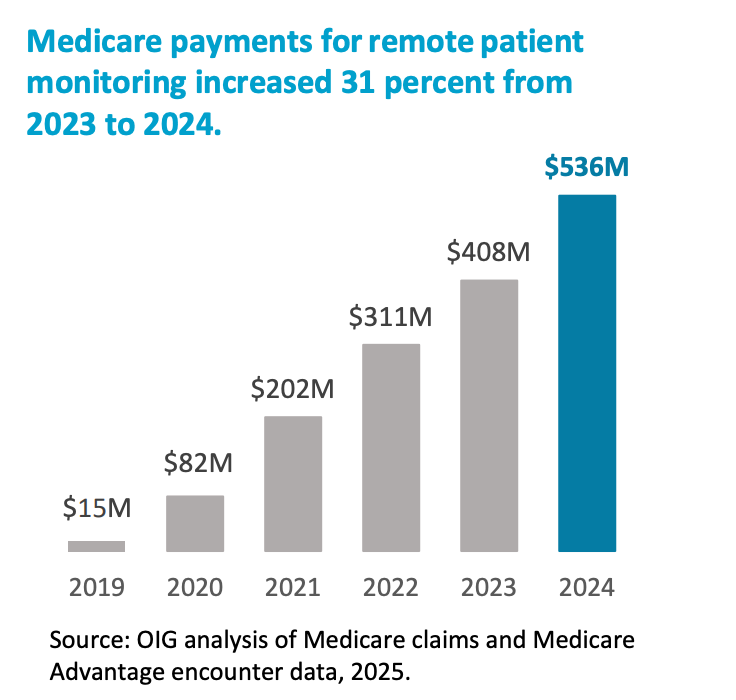
The Division of Well being and Human Providers Workplace of Inspector Normal (OIG) just lately carried out an evaluation to RPM invoicing and found that Medicare paid greater than $ 500 million for RPM providers in 2024. Primarily based on the findings, the OIG developed further measures designed to row waste, fraud and abuse with regard to RPM providers.
For his evaluation, the OIG Medicare Price-For service claims investigated from 1 January 2024 to 31 December 2024. The evaluation was aimed toward claims and conferences invoiced with a number of RPM course of codes.
The evaluation of the OIG confirmed that Medicare funds for RPM have seen constant progress yearly since 2019. As well as, practically 1 million Medicare -RPM's RPM in 2024, obtained a rise of 27% in comparison with 2023.
Oig said that these findings point out the necessity for extra supervision.
In an earlier report, the OIG has advisable that the American facilities for Medicare and Medicaid Providers (CMS) carry out periodic evaluation to establish suppliers who usually bill for registered individuals who don’t obtain all RPM parts.
On this report, the OIG additionally instructed that CMS ought to take steps to make sure that Medicare solely pays for the proper velocity.
It additionally suggested that CMS is working with Medicare Benefit Plans to make sure that they’ve the proper ensures.
The suggestions of the OIG additionally embrace that each one RPM providers are ordered by a physician or different certified care suppliers, in addition to the event of strategies to find out which well being information is checked.
“Using measures – akin to these on this report – to observe invoicing for exterior affected person monitoring will help shield the integrity of this system and forestall fraud, waste and abuse,” De Oig wrote within the report. “Moreover, this method CMS, Medicare Benefit organizations and different entities will help make sure that registrations get the advantage of exterior affected person monitoring, whereas on the identical time the dangers within the discipline of program -integrity dangers are minimized.”