Half 3 – Healthcare economist
See my earlier posts on IRA drug choice worth negotiations (Half 1) and producer knowledge submission (Half 2).
At this time we’ll speak in regards to the negotiation course of and the way CMS will decide the utmost truthful worth (MFP).
What would be the worth of CMS for various dosages?
“CMS will base the one worth on the price of the chosen drug per equal 30-day provide (moderately than per unit – comparable to pill, capsule, injection – or by quantity or weight-based measure), weighted throughout dosage types and strengths. .”
Is there a most worth or 'ceiling' for the utmost truthful worth (MFP) that CMS affords?
The utmost MFP quantity won’t exceed:
- An quantity equal to the sum of the plan-specific enrollment-weighted quantities
- The decrease of: the common non-FAMP in 2021 plus inflation (CPI-U) or the common non-FAMP worth in February 2025
CMS will combination the 60 quantities established for every NDC-11 for the chosen drug to calculate a single quantity – individually for every methodology – for the dosage types, strengths, and package deal sizes of the chosen drug. These quantities can then be in contrast straight, and the ceiling for the one MFP of the chosen drug (together with all dosage types and strengths) would be the decrease quantity.
Trial packs, NDCs from secondary producers, NDCs with no amount distributed, or NDCs with gross lined prescription drug prices of $0 usually are not included within the MFP calculation.
Can some claims be excluded from the MFP refund?
As soon as the MFP worth is set, there are some instances the place a producer won’t should pay the MFP refund. These embrace:
“…[justification] codes for the drug prospectively bought at or below the MFP, the place the producer and supplier have a individually negotiated reimbursement quantity that differs from the usual normal reimbursement quantity, and the declare is excluded from MFP reimbursements below part 1193(d)( 1) of the act”
CMS should justify the MFP to producers. How will she do that?
The CMS justification follows a four-step course of:
- Identification of any therapeutic options to the chosen drug. This consists of FDA-approved medication for the related indication and off-label makes use of, if included in nationally acknowledged evidence-based pointers and in a CMS-recognized compendia. CMS will start by figuring out therapeutic options throughout the similar pharmacological class as the chosen drug based mostly on properties comparable to chemical class, therapeutic class, or mechanism of motion, and can then additionally think about therapeutic options in numerous pharmacological lessons based mostly on CMS' evaluation of related info. (see query beneath).
- Measure the value of the therapeutic options. For Half D medication, that is the Complete Gross Coated Drug Price (TGCDC), internet of DIR and CGDP funds and/or the Common Retail Value (ASP) for Half B medication (or final yr's MFP, if relevant )
- Decide if the drug has a novel profit. Consider whether or not the chosen drug – relative to therapeutic options – addresses an unmet want, has a helpful impression on IRA-specific populations, and the extent to which the chosen drug represents a therapeutic advance in comparison with therapeutic options
- Additional adjustment of the provisional worth. These changes will likely be based mostly on knowledge submitted by the producer, together with: (1) R&D prices and recovered R&D prices, (2) present unit prices of manufacturing and distribution; (3) advance federal monetary assist for brand new therapeutic discovery and improvement; (4) pending and authorised patent functions or exclusivities; and (5) US market and gross sales quantity knowledge for the drug, and (6) non-obligatory producer submitted knowledge.
What knowledge does CMS use to find out therapeutic options?
“…CMS will use knowledge submitted by the first producer and the general public, FDA-approved indications, drug classification programs generally used within the public and business sectors for formulation improvement, CMS-recognized Half D compendia, usually accepted medical pointers, CMS-led literature opinions, drug or drug class opinions, and peer-reviewed research.”
How might CMS decide the preliminary worth quote?
The first approach CMS will decide its preliminary 2027 worth providing will likely be based mostly on the web worth of therapeutic options.
Nonetheless…
If the chosen drug has no therapeutic different, if the costs of all recognized therapeutic options are above the authorized ceiling for the MFP… or if there’s a single therapeutic different for the chosen drug and its worth is above the authorized ceiling for the MFP… MFP is positioned, then CMS will decide the start line for the preliminary providing based mostly on the FSS or…“Large 4 worth”…whichever is decrease. If the FSS and Large 4 costs are above the statutory ceiling, CMS will use the statutory ceiling as a place to begin for the preliminary supply.
Why has CMS chosen to set the preliminary worth based mostly on the value of therapeutic options?
Observe that CMS thought of a wide range of choices to find out the preliminary worth supply, together with internet costs, unit prices of manufacturing/distribution, home reference costs versus the Federal Provide Schedule (FSS) worth, a “truthful revenue” worth on based mostly on whether or not R&D prices have been recovered and a margin on the unit prices of manufacturing and distribution, however settled on the premise of the web worth of therapeutic options.
Nonetheless, it states that the web worth of therapeutic options – regardless of limitations – is a most popular possibility:
“In taking this method, CMS acknowledges that the value of the therapeutic different(s) for a particular drug is probably not excessive sufficient to mirror its medical profit. to start growing the preliminary providing throughout the context of the price and medical good thing about a number of medication that deal with the identical illness or situation. By utilizing the value(s) of the therapeutic options of the chosen drug, CMS can goal the preliminary providing based mostly on part 1194(e)(2) elements by adjusting this baseline relying on whether or not the chosen drug affords extra, much less or an analogous profit in comparison with the therapeutic options.”
What elements will affect CMS' choice to regulate the preliminary providing?
Some issues embrace:
- Scientific profit conferred by the chosen drug in comparison with its therapeutic different(s),
- Influence on patient-reported outcomes and affected person expertise
- Influence on healthcare suppliers
- Utilization patterns of the chosen drug versus its therapeutic different(s)
- Suggestions from consultations with physicians, sufferers or affected person organizations, educational specialists and/or the FDA
- Influence on CMS Particular Populations (People with Disabilities, the Aged, the Terminally In poor health, Youngsters, and Different Medicare Beneficiaries)
- Whether or not or not the therapy meets an unmet medical want
Key related info that will likely be thought of consists of: “…peer-reviewed analysis, professional experiences or white papers, doctor experience, real-world proof and affected person expertise.” Key outcomes to think about embrace a wide range of outcomes, together with patient-centered outcomes and affected person expertise.
Though CMS notes that it’s going to not use cost-effectiveness analyzes based mostly on QALYs, it has not commented on whether or not it might use different approaches, comparable to equal worth of life years gained (evLYG), years of well being complete (HYT), or generalized and threat -analysis. -adjusted QALYs (GRA-QALYs).
These elements will affect the value via a qualitative choice course of.
Will supplier expertise impression CMS choices?
Sure. The steering states that “CMS can also take into consideration the healthcare supplier perspective to the extent that this straight displays on the expertise or related outcomes of the affected person taking the chosen drug.”
Does CMS think about prices when assessing whether or not a therapy is a therapeutic advance?
Sure.
“CMS will decide the extent to which a particular drug represents a therapeutic advance in comparison with its therapeutic different(s) by inspecting enhancements in outcomes in comparison with its therapeutic different(s) (e.g., the chosen drug is healing versus a therapeutic different that delays delays). development) and can think about the prices of such therapeutic options. CMS could think about a particular drug to be a therapeutic advance if there may be proof that the chosen drug gives a considerable enchancment in outcomes in comparison with the chosen drug's therapeutic options for a sign(s).
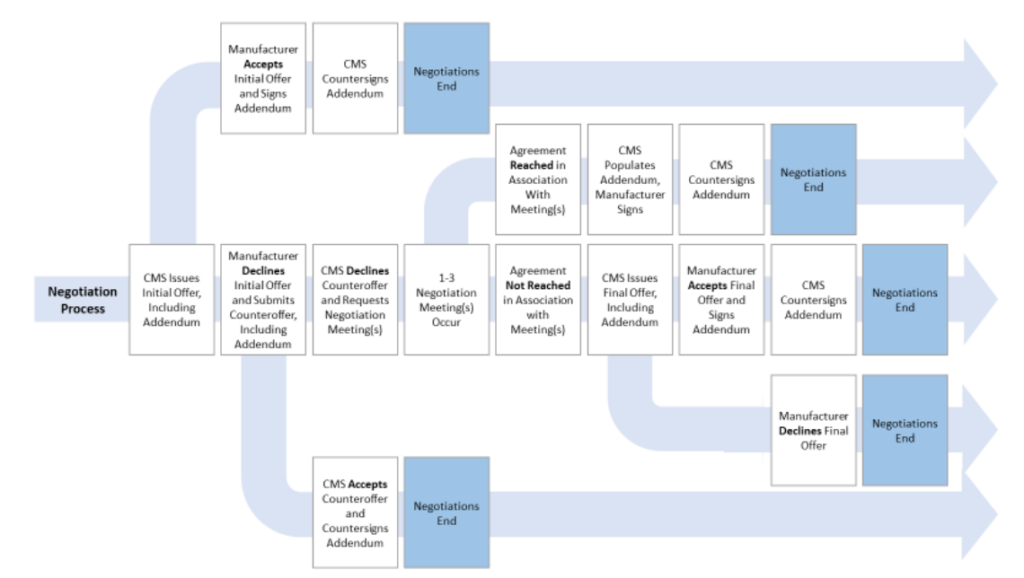
How will the negotiation course of proceed?
That is summarized within the graph beneath.
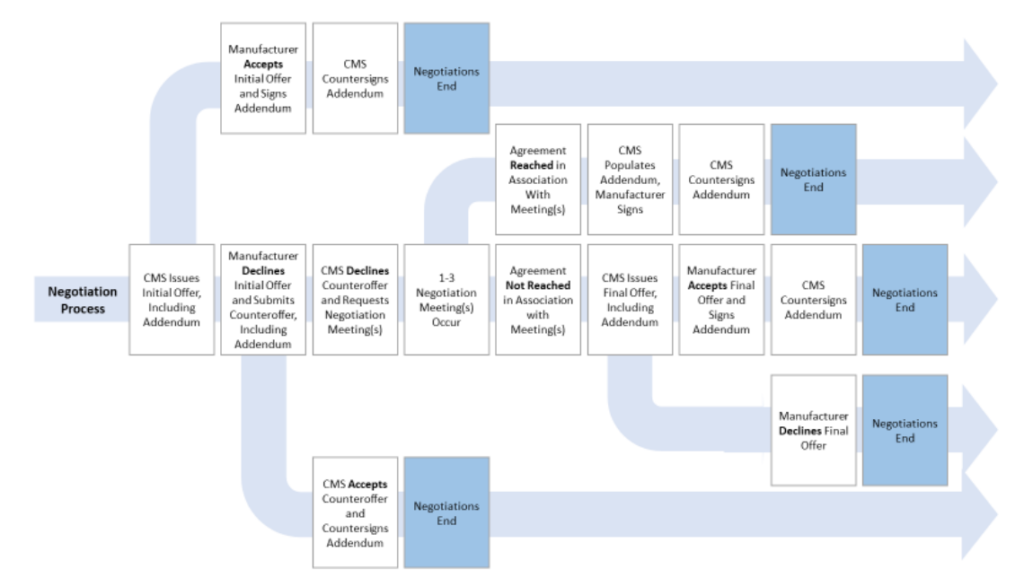
Extra particulars might be discovered within the CMS steering doc right here.